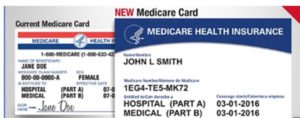
The Medicare Beneficiary Identifier (MBI) is now required for all Medicare transactions. In other words, for medical billing use of the MBI is essential. The Centers for Medicare & Medicaid Services (CMS) replaced the Social Security Number (SSN)-based Health Insurance Claim Numbers (HICNs) with the MBI and mailed new Medicare cards to all Medicare beneficiaries. The cards with MBIs offer better identity protection.
The Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) required CMS to remove SSNs from all Medicare cards. CMS replaced the SSN-based HICN with a new, randomly generated MBI. The MBI hyphens on the card are for illustration purposes: don’t include the hyphens or spaces on transactions. The MBI uses numbers 0-9 and all uppercase letters except for S, L, O, I, B, and Z. We exclude these letters to avoid confusion when differentiating some letters and numbers (for example, between “0” and “O”). The MBI specifications format is available on the CMS website.
With a few exceptions, Medicare will reject claims that Medicare providers submit with Health Insurance Claim Numbers (HICNs). Medicare will reject all eligibility transactions you submit with HICNs.
There are three methods that providers can use to obtain Medicare Beneficiary Identifiers:
1. Ask the Medicare beneficiary for their Medicare card.
2. Use them according to Medicare Administrative Contractor (MAC) secure Medicare Beneficiary Identifier lookup tool. Providers may look up MBIs for Medicare insureds when the beneficiary does not know their MBI. Medicare Advantage Plan beneficiaries are listed. The Social Security Number (SSN) is required to search for an MBI, and it may differ from the HICN, which uses the SSN of the primary wage earner.
3. Check the remittance advice – If a provider saw a patient and got a claim payment decision based on a claim submission with a HICN before January 1, 2020, the remittance advice also has the Medicare Beneficiary Identifier on every remittance advice when a provider submitted a claim with a
valid and active HICN from October 1, 2018, through December 31, 2019.
There are a few exceptions regarding the use of the Medicare Beneficiary Identifier:
- Appeals – Either HICNs or MBIs may be used for claim appeals and related forms.
- Claim status query – a HICN or MBI may be used to check the status of a claim (These are also known as EDI 276 transactions) if the earliest date of service on the claim is before January 1, 2020. If a provider is checking the status of a claim with a date of service on or after January 1, 2020, the provider must use the MBI.
- Span-date claims – You can use HICNs or Medicare Beneficiary Identifiers for 11X-Inpatient Hospital, 32X- Home Health (home health final claims and Request for Anticipated Payments [RAPs]) and 41X-Religious Non-Medical Health Care Institution claims if the “From Date” is before the end of the transition period (December 31, 2019). If a patient starts getting services in an inpatient hospital, home health, or religious non-medical health care institution before December 31, 2019, you may submit a claim using either the HICN or the MBI, even if you submit it after December 31, 2019.
How will the MBI look on the new card?
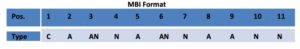
The MBI will contain letters and numbers. Here’s an example: 1EG4-TE5-MK73
- The MBI’s 2nd, 5th, 8th, and 9th characters will always be a letter.
- Characters 1, 4, 7, 10, and 11 will always be a number.
- The 3rd and 6th characters will be a letter or a number.
- The dashes aren’t used as part of the MBI. They won’t be entered into computer systems or used in file formats.
Related Topics:


